Treating severe brain injury often requires immediate surgery, including implantation of an electronic sensor that monitors tissues and fluids and digitally provides real-time information about intracranial pressure, temperature and wound healing. These devices, however, have one major drawback: eventually, they must come out, requiring an additional surgery to extract the device from the body and concomitant risk and expense.
In a recent Nature Biomedical Engineering study, a team of Northwestern scientists led by John Rogers (materials science and engineering, biomedical engineering and neurological surgery) introduces a new type of sensor, one that completely dissolves in the body when no longer needed. The study also successfully deploys a powerful, new photonics-based optical technology developed by lead author Wubin Bai, a postdoctoral fellow in John Rogers’ lab.
“This is the first time we’ve brought the ideas of biodegradable technologies into the realm of optics and photonic systems” says Rogers. “Optical characterization of tissue can yield quantitative information on blood oxygenation levels. Fluorescence signals can reveal the presence of bacteria as a diagnostic for the formation of an infection at an internal wound site. Fluorescence-based calcium imaging can reveal metrics of brain activity. There are also ways that light can be used to activate certain biological processes and that’s a next step for us.”
The work fits into a broader context of Rogers’ lab that develops materials for electronic, semiconductor or optical systems designed to go into the body, perform diagnostic and therapeutic functions, then dissolve after a pre-determined amount of time. In addition to providing critical information about physiological function, implantable sensors also can function as electrical stimulators for accelerating the rates of neural regeneration in damaged peripheral nerves, or as drug delivery agents electronically programmed to release drugs at certain time points.
From clinical needs to breakthrough solutions
“The project started with an idea that came from a discussion with professors in the clinic,” says Bai.
From skin patches worn by Gatorade-sponsored athletes to monitor rehydration needs to wireless monitors that track the vital signs of premature babies, Rogers’ team regularly collaborates with doctors and surgeons across the country to develop innovate solutions to thorny problems that arise in the clinic. He estimates that his lab has more than 20 active Institutional Review Board-approved studies of other technologies involving human subjects underway at Northwestern alone.
Rogers’ lab is looking to expand the biodegradable electronic technology to heart applications for both adults and children, in response to inquiries from Northwestern cardiologists. The doctors identified a need for a programmable sensor to monitor the oxygen level around the heart during surgery with children. They also sought solutions for a temporary pacemaker to deliver electrical stimulation, as necessary, during a recovery period following a heart surgery. After a specific time has elapsed, the devices naturally dissolve away and disappear in the body.
“One of the biggest challenges was integrating heterogeneous biomaterials together to form a functional and bioresorbable system making all of the constituents of the materials of the devices bioresorbable,” said Bai. “We had to precisely control both the composition materials’ chemistry and the device design, and dosage of each parameters together.”
Using substances naturally found in the body, the team created coating layers that dissolved very slowly. Inside, they used primarily silicon and zinc to create the functional materials for photodetection and electrical readout. The researchers then fabricated and tested three different devices useful for specific applications, all micron scale and smaller than the tip of a needle in final form. The first was composed of a silicon nanomembrane designed to detect a light at a single wavelength to monitor changes in blood flow. The second incorporated three such devices in a stack to detect multiple colors, as a simple form of chemical spectroscopy. The third contained an optical filter allowing for precise control for sensing neuron activity.
Designing the experiments
Integral to the biological aspects of the research were five experts from Chemistry of Life Processes Institute-affiliated core facilities and coauthors of the study who worked closely with Bai to plan and implement the study’s extensive in vivo proof-of-concept experiments.
Fraser Aird, PhD, and Irawati Kandela, PhD, and Iwona Stepien with the Developmental Therapeutics Core, conducted in vivo experiments to check for any immune responses in the blood to the device. The lack of immune response meant the device was not toxic to the mice. Jessica Hornick, PhD, Biological Imaging Facility, measured immune response and tissue regrowth after implantation at various timescales. Her findings concluded tissue bounced back and the device wasn’t toxic to the body. Chad Haney, PhD, and Anlil Brikha with the Center for Advanced Molecular Imaging, performed the CT imaging. CAMI’s images provided powerful physical evidence that the device disappeared slowly from week to week until it fully reabsorbed into the body. The final test was to determine whether traces of the device remained in the organs. Keith MacRenaris, PhD, Quantitative Bioelement Imaging Center, analyzed the organs throughout the experiment to measure the different concentrations of zinc and silicon, the materials used to make the device, and found these too dissipated over time.
“The core facilities have been a fantastic resource for us,” says Rogers. “Sometimes you’re working in an out-of-the-box area and it’s very much exploratory and it can be non-trivial to find collaborators with the necessary animal expertise. As a result, there can be an activation barrier for people engaged and involved. Having the cores as an additional option for collaborator-based research around the biological aspects is great thing.”
by Lisa La Vallee
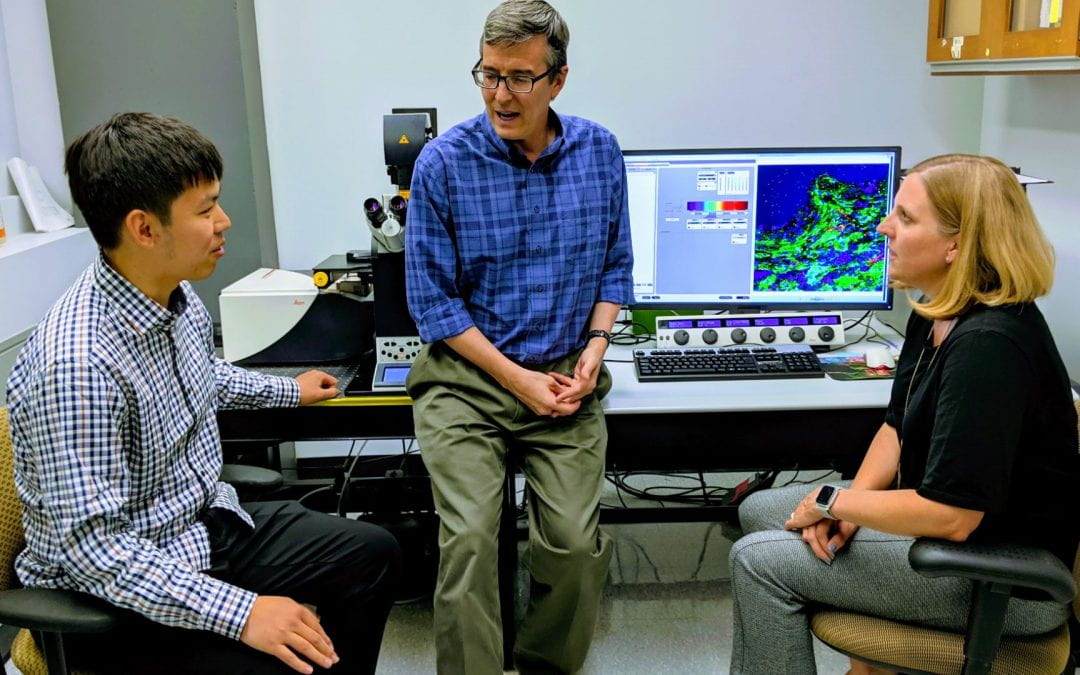
Feature image: Wubin Bai, Professor John Rogers, and Jessica Hornick huddle in the Biological Imaging Facility, a CLP-affiliated core facility that collaborated on the study.